

MBBS (AIIMS), MS (Surgery, AIIMS), MNAMS, FACS (USA), FICS (USA), FUICC
Tue, 06 Feb 2024
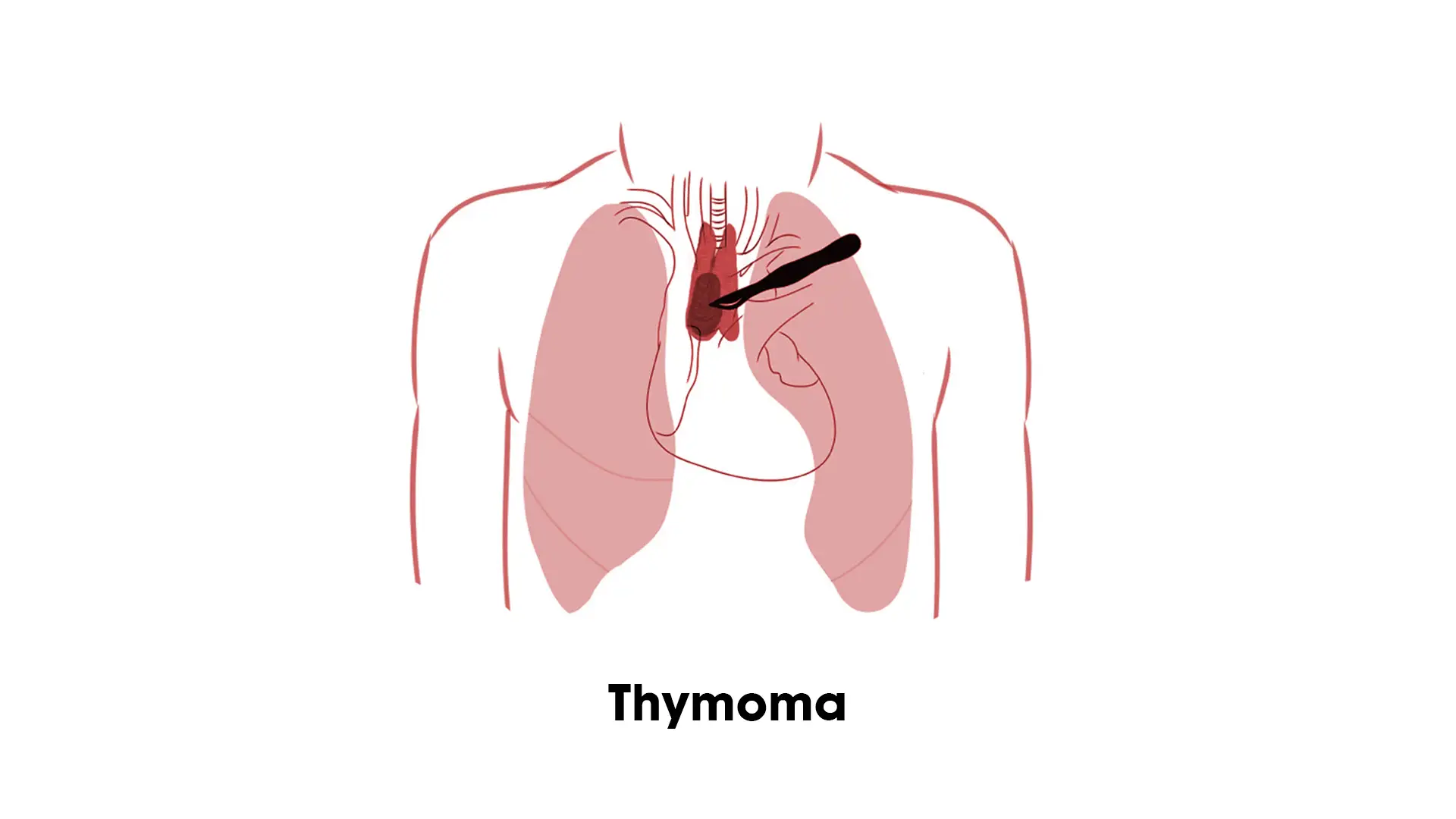
Thymoma is a rare and often misunderstood tumour that originates in the thymus, a small organ located in the chest, behind the breastbone. Thymomas are relatively uncommon, accounting for only about 1% of all mediastinal tumours.
Despite the rarity, thymoma can alter people’s quality of life and even lead to uncomfortable symptoms that are hard to manage. Having a comprehensive understanding of this disease and knowing when to see a doctor is an effective way to prevent the worst situation from happening.
This guide will explore everything one needs to know about Thymoma, its causes, symptoms, and the treatment options that Dr. Arvind Kumar specialises in.
The exact cause of thymoma is poorly understood and remains a topic of ongoing research. However, several factors have been associated with the development of thymomas, including:
Some cases of thymoma are sporadic and aren’t dependent on any of the causes we mentioned above.
Since thymoma is quite a rare form of tumour and cancer, many patients don’t even realise the indicative symptoms until its too late. Most of these symptoms are common and are often not taken seriously, which means that if you notice a frequent recurrence, it is crucial to see a specialist without question.
Some of the symptoms worth prioritising are:
If you or someone you know is experiencing persistent or unexplained symptoms, seeking medical evaluation and diagnosis is crucial.
The diagnosis of thymoma involves clinical evaluation, imaging studies and pathological examination. The following are the typical steps in the diagnostic evaluation:
This is when you visit a specialist with the complaint of recurrent symptoms. The specialist will first listen to the symptoms, assess the medical history and then perform and physical examination for signs and symptoms such as chest pain, cough, difficulty breathing, etc.
For further clarity on what’s wrong, the specialist will prescribe imaging tests, including chest X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI).
Once the imaging tests confirm the presence or growth of thymoma, the next step is conducting a biopsy to collect a tumour sample to determine its type and aggressiveness.
An early diagnosis helps with an early administration of the required treatment so that the patient has a higher chance of remission after the treatment.
Surgical interventions are considered the primary route when treating thymoma, especially for patients in the earlier stages. The specificity of the administered treatment depends on the size, location, and stage of the thymoma.
This is a surgical procedure that involves complete removal of the entire thymus gland. It can be done via open surgery or minimally invasive methods such as video-assisted thoracoscopic surgery (VATS). The choice of approach depends on individual factors, such as tumour size, location, and the patients overall health.
In some cases where the thymoma is more severe and aggressive, an extended thymectomy is done to remove not only the thymus gland but also the adjoining tissues and lymph nodes to reduce recurrence in the future.
This is similar to extended thymectomy, where the thymus gland and invaded surrounding tissues are removed, too. The surgery may involve resecting parts of the lung or other structures.
Besides surgical interventions, thymoma patients might undergo non-surgical procedures like radiation therapy and chemotherapy as adjuvant treatments to reduce the patients recurrence risks. Generally, these are advised in patients with advanced stages of thymoma.
Surgical approaches to removal of the thymus
The Thymus gland is centrally located in the upper body and especially its nearness to the heart, the thymus presents specific challenges for surgery. In fact, there are occasions when the thymus may be removed simply to provide unobstructed access to certain segments of the heart during cardiac surgery.
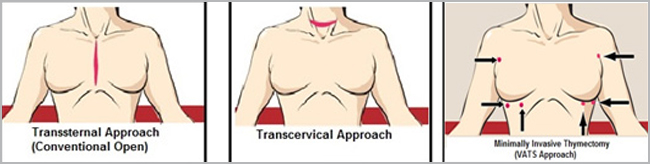
Transsternal Approach (Conventional Open) which involves cutting through the sternum or breast bone. Sometimes referred to as cracking the chest, which is essentially the same approach used for open heart surgery. It is reserved for very large thymomas or those that have invaded nearby structures.
Transthoracic, (Minimally Invasive Thymectomy /VATS Thymectomy/ Thoracoscopic Thymectomy) which approaches the thymoma through multiple small incisions on one or both sides of the chest. In VATS (Video Assisted Thoracoscopic Surgery) Thymectomy, a video camera is used to see the surgical field, in this case the thymus and surrounding tissue. This type of procedure generally uses small incisions in the chest for the camera, surgical instruments. The approach is sometimes called Minimally Invasive Thymectomy.
More About Thymoma
With the advent of robotic surgery, which is truly minimally invasive one can achieve the effectiveness of a transsternal approach without the trauma associated with going through the breast bone. In Robotic Thymectomy, the surgeon sits at the console and operates using miniaturised instruments with highly flexible joints to perform the most delicate aspects of a thymectomy in a very precise manner. Guided by a high resolution, three-dimensional thoracoscopic view, the operating surgeon can visualize the entire thymus.
This can be crucial, especially to see the exact position of the thymus tissue and avoid cutting the nearby crucial structures. Good vision is also essential for completely dissecting the thymic horns, the top portion of the thymus that extends into the neck. In particular, the combination of the surgeon controlled camera, the computer enhanced clarity of the image, and the dexterity of the miniaturized robotic surgical instruments easily overcome the tight operating space around the thymus and provide the precision necessary to safely navigate a complete thymectomy.
However not all thymomas are fit for robotic surgery. It depends on the tumour size, its invasiveness and experience of the surgeon. Dr. Arvind Kumar, having performed over 200 thymectomy by robotic method, has the countrys largest experience in performing robotic thymectomy.
Radiotherapy therapy Thymoma and Thymic carcinoma: Radiation therapy is a type of cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing.
Chemotherapy Thymoma and Thymic carcinoma: Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). The way the chemotherapy is given depends on the type and stage of the cancer being treated.
Chemotherapy may be used to shrink the tumor before surgery or radiation therapy. This is called neoadjuvant chemotherapy.
Thymoma is a rare and complex tumour that can spread quickly and lead to irreparable damage if early diagnosis and treatments aren’t administered to the patient. Due to the situations sensitivity, diagnosed patients must work with skilled and experienced specialists like Dr. Arvind Kumar, who has treated such patients with the most appropriate treatment plan.
If you are experiencing recurrent symptoms that align with thymoma or know someone who is, kindly contact us directly for appointments.
Copyright @ (Prof.) Dr. Arvind Kumar. All Rights Reserved / Thoracic Surgical Oncologis
License Number: U.P State Medical Council (India) No. 27637
